Kitware: Leading-Edge Ultrasound Research
Ultrasound has become a catalyst for innovation, new insights, and improved methods in a wide range of clinical procedures and medical research applications. A longstanding centerpiece in the practice of obstetrics, cardiology, and radiology, ultrasound research and development activity has surged in the past few years. This surge is evident in the double-digit growth rate of the portable ultrasound device market in non-traditional specialties, e.g., anesthesiology, musculoskeletal, and emergency medicine [1].
TRENDS • ULTRASOUND RESEARCH PROJECTS • COLLABORATION • ADDENDUM
Kitware is on the leading-edge of ultrasound research and development. Working with academic and industrial pioneers, we are laying the groundwork for next-generation devices that will generate cost-savings for the healthcare system and, most importantly, save lives. In particular, we are focusing on approaches that enable low-cost yet highly capable ultrasound equipment to be used in a broad range of clinical contexts by relatively less experienced medical personnel. We envision ultrasound becoming the stethoscope of the future—pervasive in doctors offices, ambulances, and clinics around the world; however, this future will only be achieved if the necessary expertise can be embedded within the algorithms and user interfaces of those highly portable ultrasound probes.
TRENDS
Four trends that are forming within the field of medical ultrasound research are as follows:
Trend #1: Measurement Automation
Fully realized, this trend will make it possible for users with almost no experience to deploy ultrasound imaging in multiple settings. The benefits will include 1) reduced costs to the healthcare system by targeting novice users as well as in-field, in-home, pre-hospital and bedside (i.e., “point-of-care”) applications; 2) better patient outcomes, as imaging can be obtained earlier in (e.g., at the scene of an accident, for patient triage) and more frequently during the disease course; and 3) improved measurement standardization and inter-user reliability.
Trend #2: Multi-modality and Longitudinal Image Fusion, in the Presence of Pathologies
The roles of fluoroscopy, computed tomography (CT), and magnetic resonance imaging (MRI) are well established for diagnosis and surgical planning; however, these baseline images can only be acquired prior to or intermittently during surgeries and treatments. This leaves the clinician to work with planning images that become increasingly irrelevant as the disease progresses or as the surgeons move or remove anatomical structures. Ultrasound, which can track real-time anatomical changes, can serve as a bridge between baseline images and the current conditions of the patients.
Trend #3: Computer-Assisted Ultrasound Probe Placement
Determining where to place an ultrasound probe and how to move that probe to view a particular anatomic structure requires significant training and expertise. Such trained experts are frequently not available for point-of-care applications. Novel three-dimensional (3D) tracking technologies and image analysis methods are being integrated to provide real-time estimates of the anatomic location of an ultrasound probe, and robotic systems are being devised to automate probe placement for clinical and research applications, to bolster repeatability and efficiency.
Trend #4: Intervention Guidance
Those in the healthcare field will tell you that needle guidance is among the more procedurally frustrating aspects of their jobs. On average, three attempts are required to successfully find an artery/vein and insert the needle, and failure isn’t as innocuous as you may believe. It can lead to hematomas, nerve damage, or infection. Ultrasound is quickly becoming an established instrument for vessel localization, and emerging companion software, including augmented reality visualization systems, are being developed to further simplify this procedure.
ULTRASOUND RESEARCH PROJECTS
The following projects are a representative subset of the ongoing, ultrasound-based research and development being led or supported by Kitware. These projects range from cancer research to surgical planning. Kitware’s open-source philosophy spurs innovation, collaboration, and development in these exciting ultrasound augmentation efforts.
1. Computer-Augmented Point-of-Care Ultrasound: Pre-hospital E-FAST and Traumatic Brain Injury Exams
For the full potential of point-of-care ultrasound (POCUS) to be realized, it must be treated as a new modality, not simply as an inexpensive, portable ultrasound system. POCUS must involve automated data analyses, rugged hardware, and specialized interfaces to guide novice users to properly place and manipulate an ultrasound probe, gather high-quality data, and interpret the returned ultrasound data. In particular, the output of a POCUS system should typically be quantitative measures and easy-to-understand reformulations of the acquired data, not B-mode images; it should be assumed that the expertise needed to interpret B-mode images will not be readily available at point-of-care. Example POCUS applications include detection of intra-abdominal bleeding by EMS personnel for patient triage at the scene of an accident, diagnosis of increased intracranial pressure by medics using the computer-assisted measurement of optic nerve sheath diameter, and monitoring of liver tissue health in the homes of at-risk patients.
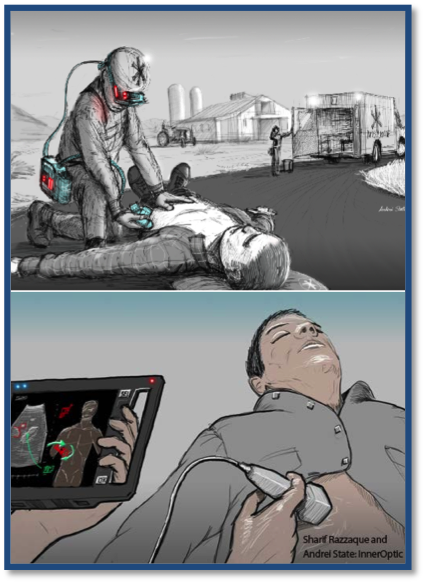
The extended focused assessment with sonography for trauma (E-FAST) exam is a means to triage patients who may have a pneumothorax (collapsed lung) or internal bleeding due to abdominal trauma. By assessing select areas on the patient’s body with ultrasound, valuable information is provided that can help determine whether a patient is destined for observation, CT scanning, or the operating room. Unfortunately, while the cost of portable ultrasound systems continues to drop, the training required remains a major hurdle. Studies have shown that E-FAST is effective in pre-hospital settings [2]; however those studies have involved physicians and surgeons with up to 100 hours of specialized E-FAST training, and such extensive training isn’t practical for typical EMS personnel. The reality is that it has been estimated that the rate of preventable trauma-related deaths is 85% higher in rural populations than in urban populations [3], with pre-hospital patient care being an urgent and unmet need in rural and under-served populations [Trauma.org].
What can be done to bring the powerful diagnostic capabilities of ultrasound to the masses at the scene of accidents and natural catastrophes? Kitware is helping to spur the widespread adoption of trauma-focused ultrasonography by creating a portable and easy-to-use system that integrates (1) advanced machine learning methods with (2) low-cost ultrasound probes from Interson and (3) innovative augmented reality displays from InnerOptic. Aspects of this effort are being funded by the NIH and spearheaded by clinical collaborators in Trauma Surgery and Emergency Medicine at Washington University in St. Louis and at Duke University in North Carolina.
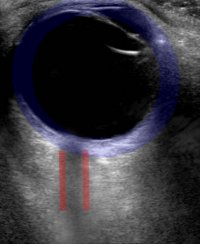
Our work in this area has also been extended to include the in-field assessment of traumatic brain injury (TBI) by using ultrasound to assess the dilation of the optic nerve, an immediate indicator of increased intracranial pressure associated with TBI.
A recent highlight of our work is the workshop on point-of-care ultrasound that we organized at the 20th international conference on Medical Image Computing and Computer-Assisted Intervention (MICCAI 2017). The proceedings of our workshop, including papers from Kitware, have been published by Springer as part of their Lecture Notes in Computer Science series. Our publications at that and other workshops, conferences, and journals include the following:
- S. Gerber, M. Jallais, H. Greer, M. McCormick, S. Montgomery, B. Freeman, D. Kane, D. Chittajallu, N. Siekierski, S. Aylward, “Automatic Estimation of the Optic Nerve Sheath Diameter from Ultrasound Images”, in Imaging for Patient-Customized Simulations and Systems for Point-of-Care Ultrasound, LNCS 10549, 2017
- M. Jallais, H. Greer, S. Gerber, M. McCormick, D. Chittajallu, N. Siekierski, S. Aylward, “Ultrasound Augmentation: Rapid 3-D Scanning for Tracking and On-Body Display” in Imaging for Patient-Customized Simulations and Systems for Point-of-Care Ultrasound, LNCS 10549, 2017
- S. Aylward, S. Gerber, M. McCormick, M. Jallais, S. Montgomery, L. Kohli, B. Freeman, S. Kane, “Point-of-care ultrasound for detecting elevated intracranial pressure in the field” Special Operations Medical Association’s Scientific Assembly (SOMSA) 2017 (Podium Presentation)
- S. Aylward, M. McCormick, M. Jallais, S. Gerber, S. Montgomery, L. Kohli, B. Freeman, S. Kane, “Computer-Assisted FAST exam for in-field triage” SOMSA 2017 (Poster Presentation)
- X. Han, X. Yang, S. Aylward, R. Kwitt, M. Niethammer, “Efficient Registration of Pathological Images: A Joint PCA/Image-Reconstruction Approach” IEEE International Symposium on Biomedical Imaging, Melbourne, Australia, 2017
- S. Aylward, M. McCormick, HJ. Kang, S. Razzaque, R. Kwitt, M. Niethammer, “Ultrasound Spectroscopy” Proceedings of the International Symposium on Biomedical Imaging (ISBI), Prague, 2016 (Presentation)
We have also given a variety of invited talks on the blending of open science and point-of-care ultrasound. The low-cost ultrasound probes of point-of-care ultrasound have invigorated a grass-roots industry that is undergoing rapid growth thanks, in part, to its adoption of open science practices, e.g., promoting open APIs, using and contributing to open-source software, and encouraging and benefitting from collaborations between academia and industry. Slides from select talks are offered below:
- New Horizons: The Future of Medical Ultrasound, Berlin, Germany (2018.01.17-Aylward-NewHorizons.pdf)
- Vanderbilt University (2017.11.01-Vanderbilt-Aylward.pdf)
Similar talks were given at
- The University of Pennsylvania
- Robarts Research Institute
- Johns Hopkins University
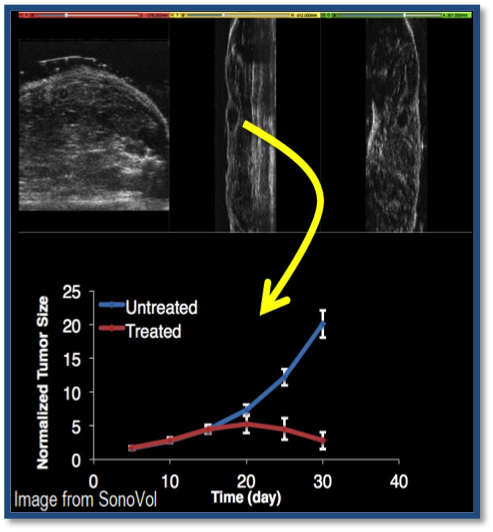
2. Ultrasound Analysis of Tumor Micro-environment
With the University of North Carolina at Chapel Hill and SonoVol, a pre-clinical ultrasound startup, Kitware is participating in the development of tools and technologies to help cancer researchers track tumors in animal models. One biomarker of cancer malignancy is tortuosity of vessels within the tumor—an indicator of how well the tumor is nourished. One goal of our collaboration is to monitor tumor vessels with high-frequency ultrasound and advanced image-analysis algorithms, enabling researchers to investigate how tumors respond to potential anti-cancer drugs. This project is funded by the NIH and NSF, with grants to Kitware, UNC, and SonoVol. Once realized, this approach will facilitate drug development and help researchers in academia and industry identify promising therapies earlier.
Related publications
- SE. Shelton, BD. Lindsey, R. Gessner, Y. Lee, S. Aylward, H. Lee, E. Cherin, F. Stuart Foster, PA. Dayton, “Acoustic angiography: a new high-frequency contrast ultrasound technique for biomedical imaging.” Proc. SPIE 9871, Sensing and Analysis Technologies for Biomedical and Cognitive Applications 2016, 987109 (May 19, 2016); doi:10.1117/12.2229179.
- R. C. Gessner, S. R. Aylward, and P. A. Dayton, “Mapping Microvasculature with Acoustic Angiography Yields Quantifiable Differences between Healthy and Tumor-bearing Tissue Volumes in a Rodent Model,” Radiology, vol. 264, no. 3, pp. 733–740, 2012.
3. Ultrasound Augmentation: Peripheral Vascular Access
Kitware is developing an innovative augmented reality system and building upon their extensive expertise with vessel modeling to locate veins in a patient, compute the path for a needle to reach a vein, and then interactively instruct the clinician on how to move the needle to make it follow the computed path.
One particularly innovative aspect of the system is that it provides guidance to the clinician via an integrated pico projector that displays the location of the vein and needle guidance instructions directly on the patient’s skin. Once fully developed, this will bring subcutaneous anatomy and instruments to the surface, making imprecise needle sticks a thing of the past. Collaborators for this project are Interson, InnerOptic, Duke University, and Washington University in St. Louis.

Related Publications
- R. Kwitt, DF. Pace, M. Niethammer, S. Aylward, “Studying Cerebral Vasculature Using Structure Proximity and Graph Kernels.” MICCAI (2) 2013: 534-541
- R. Kwitt, N. Vasconcelos, S. Razzaque, S. Aylward “Recognition in Ultrasound Videos: Where Am I?” MICCAI (3) 2012: 83-90
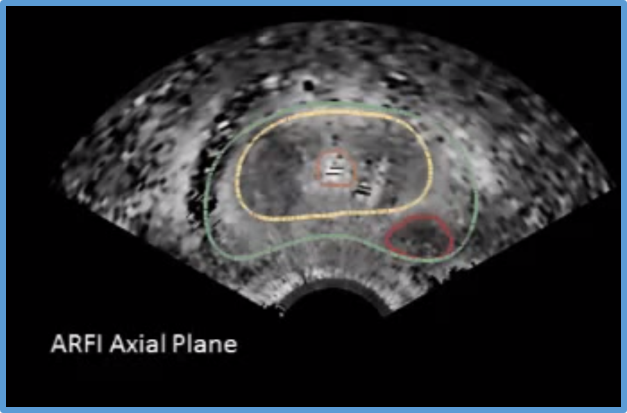
4. Ultrasound and mpMRI Fusion for Prostate Malignancy Assessment
An effective, non-invasive malignancy assessment of common prostate lesions can prevent unnecessary surgical removal of the prostate. Via a subcontract from Duke University on an NIH-funded grant, Kitware is registering MRI images with multiple novel ultrasound imaging modalities with the goal of improving the standard of care for prostate cancer.
5. Ultrasound in Jaw Correction Surgery
During jaw correction surgery, the condyle can dislocate in the temporomandibular joint. Such dislocations can be difficult to detect and even more difficult to correctly fix during surgeries.
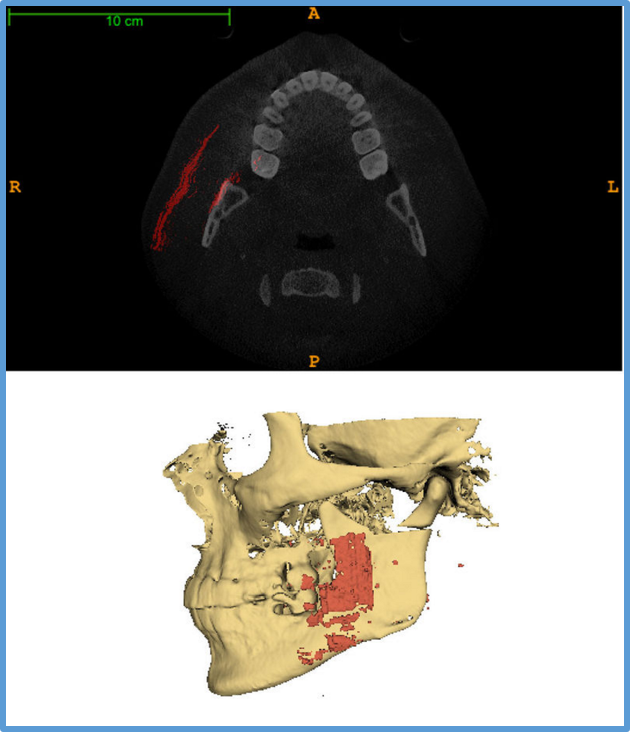
With a grant from the NIH, the Denofacial Deformities Clinic at The University of North Carolina at Chapel Hill is funding Kitware to develop ultrasound-to-CT registration methods that can help intra-operatively detect the occurrence of and guide the correction of these dislocations. This work also features ultrasound segmentation techniques, novel visualization methods, and high-precision ultrasound probe tracking technologies.
COLLABORATING WITH YOU
The projects listed above and numerous other commercial and academic collaborations have created a synergy of expertise, software infrastructure, and innovation for ultrasound research and development at Kitware.
To learn more about how your company or research group can leverage Kitware’s ultrasound and medical computing expertise, please contact Stephen Aylward or Matt McCormick via kitware@kitware.com.
ADDENDUM
Here is some information on the Kitware team, as well as blog posts; societies, workshops, and conferences; open-source software; grant funding; and collaborators.
The Kitware Team (Alphabetic listing)
- Stephen Aylward
- Deepak Chittajallu
- Sam Gerber
- Hastings Greer
- Forrest Li
- Matt McCormick
Blog posts
Links to other blog posts on the ultrasound activities at Kitware are available here.
Societies, Workshops, and Conferences
Societies, workshops, and conferences that promote ultrasound algorithms and applications, and that are supported by Kitware, include
- Medical Image Computing and Computer-Assisted Intervention (MICCAI) Society
- MICCAI 2017 Workshop: Point-Of-Care Ultrasound: Algorithms, Hardware, and Applications
- Information Processing in Medical Imaging (IPMI) Conference 2017
- IEEE International Symposium on Biomedical Imaging (ISBI) 2017
Open-source Software
Many of the methods discussed on this page and in our other medical imaging blogs are available as open-source software via 3D Slicer and ITK. Visit the KitwareMedical and Kitware communities on GitHub to access the majority of our software.
Grant Funding
This work was supported, in part, by the following grants (in addition to several commercial contracts):
- NIH/NIGMS/NIBIB: “Slicer+PLUS: Collaborative, open-source software for ultrasound analysis” (Aylward, Fichtinger) R01EB021396: 2016-2020
- NIH/NINDS: “Multimodality image-based assessment system for traumatic brain injury” (PI: Aylward) 1R41NS081792: 2014-2017
- NIH/NIBIB: “In-field FAST procedure support and automation” (Aylward) 1R43EB016621: 2014-2015
- NIH/NCI: “Micro-tumor detection by quantifying tumor-induced vascular abnormalities” (PI: Dayton – UNC) 1R01CA170665: 2012-2016
- NIH/NCI: “Quantitative ultrasound analysis of vascular morphology for cancer assessment” (PI: Dayton, Aylward – UNC) 1R43CA165621: 2012-2016
- NIH/NCI: “Image Registration for Ultrasound-Based Neurosurgical Navigation” (PI: Wells, Aylward – BWH)
1R01CA138419: 2010-2014
Collaborators
We are thankful for the outstanding individuals and groups who have contributed significantly to the direction and developments that have been the foundation of our work, including (in alphabetical order)
- Emad Boctor, Ph.D., Johns Hopkins University
- Kevin Cleary, Ph.D., Children’s National Medical Center
- Bradley Freeman, MD, Surgery, Washington University
- Gabor Fichtinger, Ph.D., Queen’s University, Canada
- Luv Kohli, Ph.D., CTO, InnerOptic
- Sean Montgomery, MD, Surgery, Duke University
- Deborah Shipley-Kane, M.D., Emergency Medicine, Washington University
- Tamas Ungi, Queen’s University, Canada
Originally published Jan. 26, 2016
Last updated January 26, 2018
[1] Analysis of the U.S. Medical Ultrasound Imaging Systems Market Growth to be Driven by Emerging Market Segments (2011). Frost &Sullivan.
[2] Nelson BP, Chason K, “Use of ultrasound by emergency medical services: a review” Int J Emerg Med. 2008 Dec; 1(4): 253–259.
[3] Gamm LD, Hutchison LL, Dabney BJ, and Dorsey AM, eds., Rural Healthy People 2010: A Companion Document to Healthy People 2010, Vol. 1. (College Station, Texas: The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center, 2003.)
10 comments to Kitware: Leading-Edge Ultrasound Research